External transducers are still widely used today for pressure monitoring in critical care, particularly in neuro and cardiovascular health. However, this method can introduce errors due to factors like air bubbles, fluid resistance, or line compliance, which can dampen or distort the pressure signal.
Similarly, health care largely relies on magnetic resonance thermometry (MRT) to monitor tissues’ temperature. While MRT can target specific tissues, its accuracy may be affected by factors like motion artifacts (from respiration or blood flow) and tissue heterogeneity.
Why can external transducers introduce unreliable and inaccurate pressure measurements?
External transducers measure pressure using a fluid-filled line to transmit pressure from inside the body (e.g., an organ or blood vessel) to an external transducer.
External transducers can introduce several errors when measuring pressure, primarily due to the properties and handling of the fluid-filled system.
- Air bubbles in the fluid line absorb pressure waves, dampening rapid pressure fluctuations, distorting waveforms, and reducing the overall accuracy of the pressure signal.
- Clots, debris, bending, or kinking of the catheter or line may lead to complete or partial obstruction, causing false low or zero readings and leading to wrong decision-making based on poor information.
- Physical movement of the catheter, tubing, or transducer caused by patient repositioning, line adjustments, or nearby activity can introduce transient pressure spikes or oscillations unrelated to the actual physiological pressure.
- Incorrect leveling of the transducer relative to the patient’s reference point (e.g., heart level) may cause overestimation (if the transducer is below the heart) or underestimation (if above the heart) of pressure.
What are MRT’s limitations in temperature measurement?
MRT is a non-invasive imaging technique that uses the principles of magnetic resonance imaging (MRI) to measure temperature changes in tissues. Although non-invasive, the technique also comes with some limitations:
- Indirect Measurement: MRT infers temperature based on signal changes, which may introduce variability in absolute accuracy.
- Relative measurement: MRT provides temperature distribution averaged over a region rather than a single-point measurement at a specific location.
- Radiator Effect: MRT uses radio frequency (RF) fields to excite tissues. Wires can absorb RF energy, converting it into heat, which increases local temperature and leads to overestimated readings.
These risks of relying on inaccurate data may go beyond the diagnostic challenges. Patients may receive ineffective or unnecessary treatments, potentially leading to complications or hospital readmission. Not only can it compromise patient outcomes, but it also places additional strain on healthcare systems, resulting in increased costs, treatment delays, and longer waiting lists for other patients.
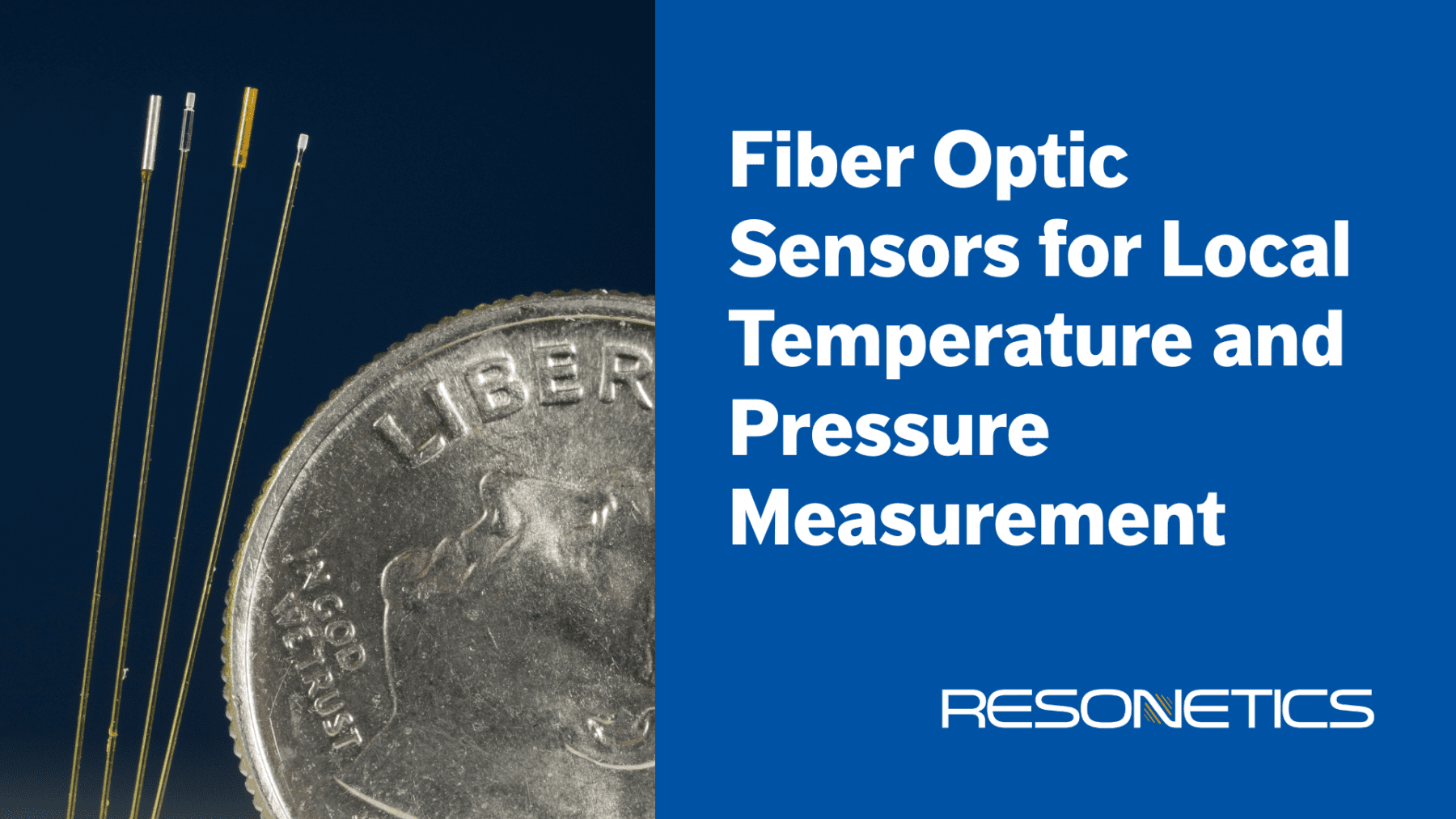
Resonetics Redefines Standards for Reliable, Accurate Measurement
Pioneer in its field, Resonetics (formerly FISO) has developed unique fiber optic sensing technologies to measure pressure and temperature locally, at the precise position where the information is required for diagnosis and treatment. Fiber optics allow Resonetics’s customers to take accurate, repeatable measurements directly at the source rather than relying on more error-prone techniques.
Why a local temperature and pressure measurement is more reliable and accurate?
Local accuracy at the site of interest: Measuring temperature and pressure directly at the organ, vessel, or tissue site ensures the most reliable and accurate results, eliminating the need for assumptions or indirect correlations associated with external techniques.
Fast response: Fiber optic pressure sensors enable quicker, instant dynamic responses because light travels faster than pressure waves propagate. Therefore, if rapid action is required, such as stopping an injection or aspiration, the system can respond more effectively and swiftly, reducing the risk of injury to the patient’s organs.
Ease of installation: Fiber optic sensors enable simple connections, allowing users to add, remove, and reconnect sensors without distance limitations. In contrast, fluid-filled lines require managing water and eliminating air bubbles, making the process more challenging.
Ease of use: No preparation work that may vary from user to user is required. The medical team simply needs to position the catheter with the fiber optic pressure sensor, after which they can proceed with diagnosis or treatment.
Precise thermal mapping: Fiber optic sensors can measure multiple distinct points as close as 1 mm apart within the same area. For example, they can monitor temperatures inside, at the edge, and outside a tumor, ensuring complete ablation of cancer cells while preserving surrounding healthy tissue.
Benefits for Health Systems and Patients
Resonetics’s fiber optic sensors provide the most reliable and accurate local temperature and pressure measurements for medical applications. They deliver direct, real-time data at the site of interest, enabling doctors to monitor the organs’ immediate response to treatment.
Consequently, using Resonetics sensors reduces errors, minimizes external influences, and enhances treatment precision, making them essential for diagnosing and managing critical conditions with increased safety and effectiveness.
- No measurement delay
- No risk of obstruction
- No signal distortion
- No distance or disconnection limit
- Better control and efficiency in diagnosis and treatments
- Improved decision-making for treatment
- Reliability in critical situations and feedback for immediate intervention
Interested in learning more? Visit Fiber Optic Sensors | Resonetics and watch DeviceTalks Tuesdays Webinar: Medical Sensors – Resonetics





